Alzheimer’s disease (AD) has been shrouded in mystery for far too long, and a recent scandal involving falsified key research only added to the confusion. But don’t be fooled – this setback only affected a small portion of the many amyloid species, and the prior decades of research remain solid. The amyloid hypothesis is still very much alive and kicking.
AD is a progressive brain disease that affects memory, thinking, and behavior. Despite being discovered over a century ago, its cause remains unknown, and only aging, family history, and head trauma are known risk factors.
β-Amyloid & Alzheimer's Disease
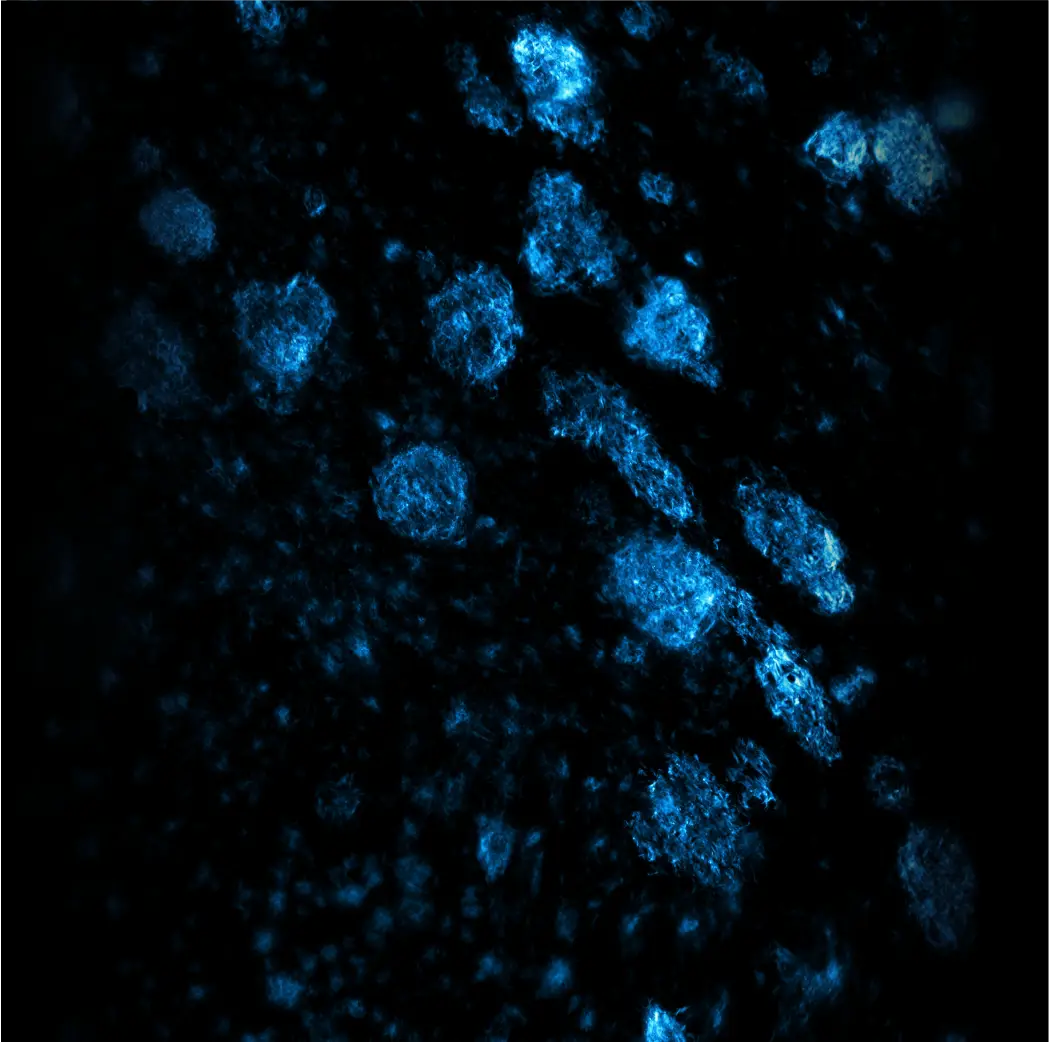
The misfolding of amyloids leads to the formation of protein tangles and insoluble fibrous aggregates, and β-amyloids, among other precipitated proteins, are closely associated with the monster that is AD. Research suggests that β-amyloids may trigger immune cells to ignite inflammation and consume neurons that have lost their function.
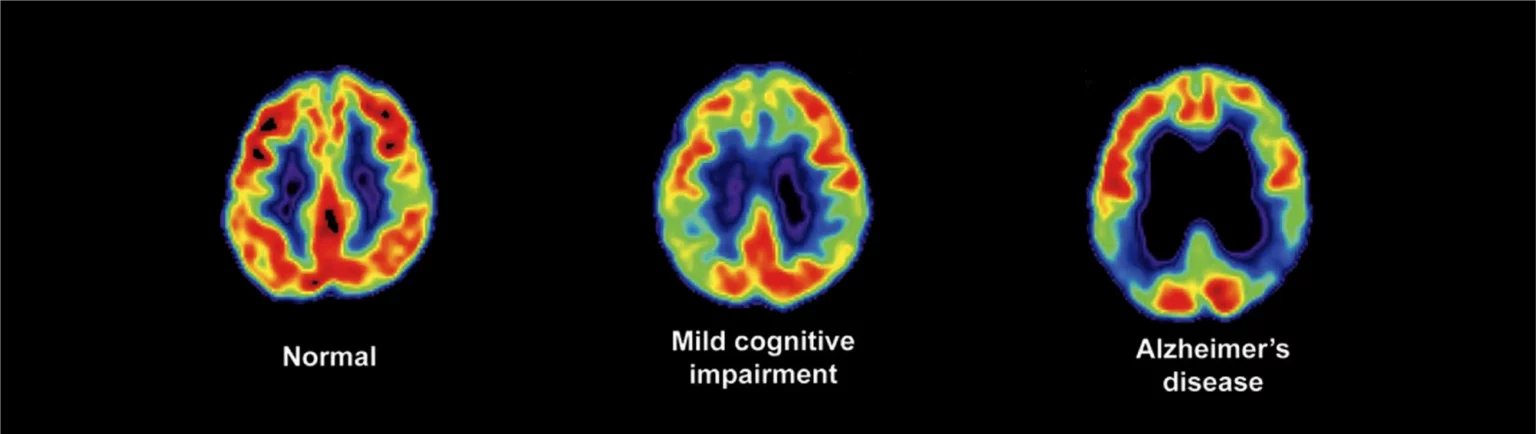
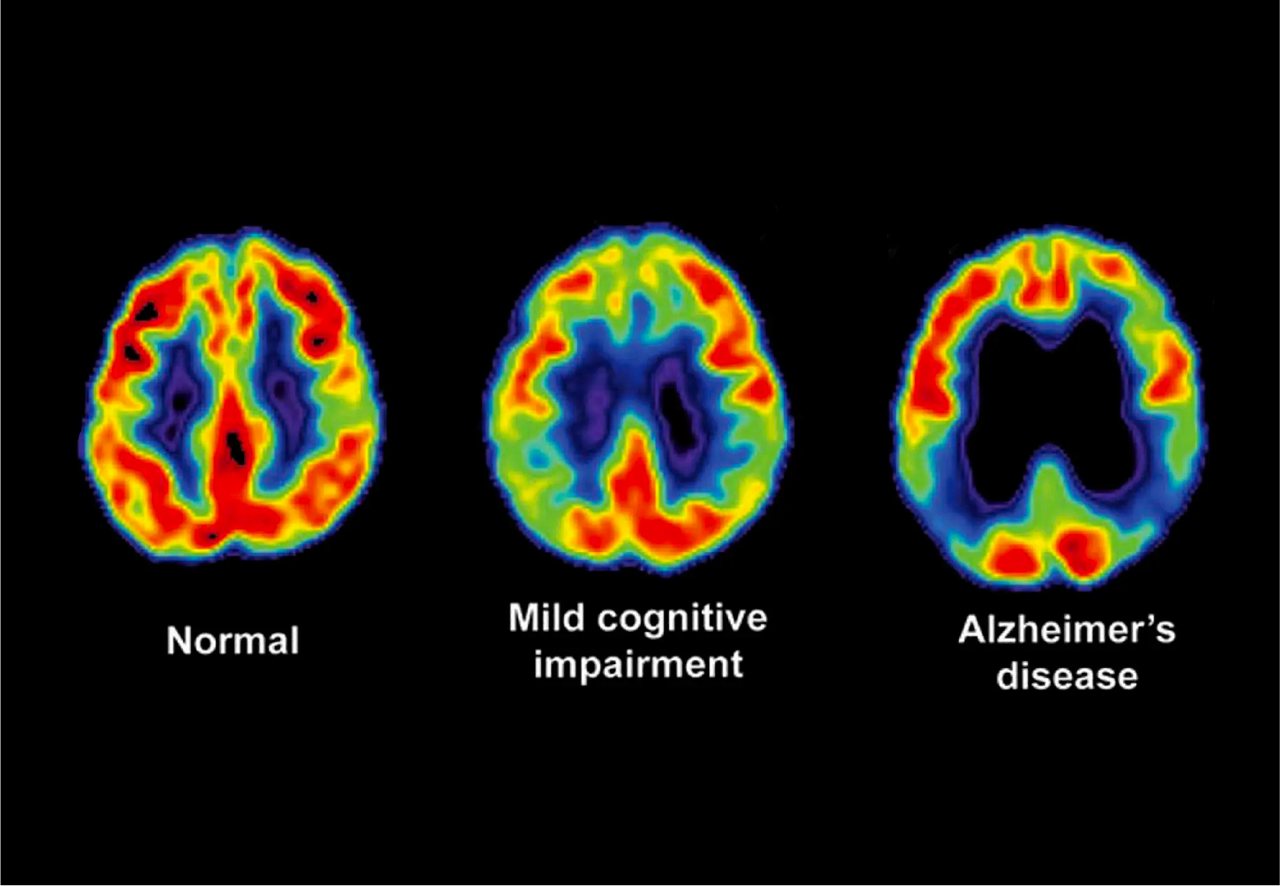
The deposits of these amyloid plaques and abnormal phosphorylation of TAU proteins cause damage and death to neurons, leading to a shortage of the neurotransmitter acetylcholine in the brain. As a result, brain cells shrink and the ventricles enlarge, with the cortex, hippocampus, and amygdala, all related to cognition, memory, and emotions respectively, being particularly affected.
The race is on to slay this monster, and researchers are leaving no stone unturned in their quest to find its main cause. Despite being an irreversible and incurable disease, improvements in early detection hold the key to improving patient outcomes.
β-Amyloid
How 3D Tissue Imaging Differs from Traditional Tissue Slice Techniques
Unraveling the mysteries of Alzheimer’s disease has been a challenge due to its unknown etiology. β-amyloid has become a classic pathological marker in the quest to understand the disease. However, traditional tissue slice techniques have limitations such as slice thickness, limited slice quantity, and human errors that may cause biased pathology image presentation and analysis.
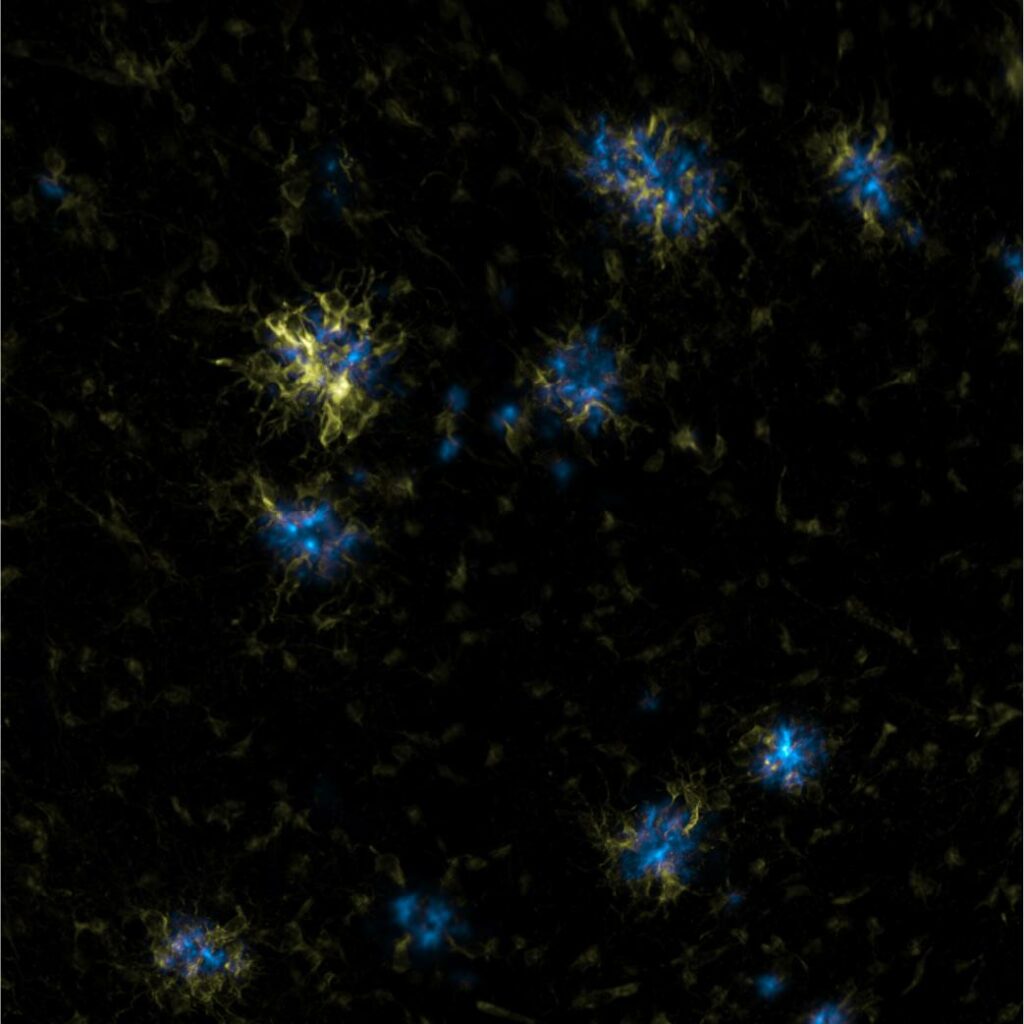
In this regard, 3D whole tissue imaging technology, such as Nebulum 3D Whole Tissue Imaging, can help researchers observe complete and continuous signals, especially in the early stages of protein deposition. This technology can also provide a better understanding of the relationship and expression of β-amyloid and microglia, which are immune cells that play a critical role in neuroinflammation in Alzheimer’s disease.
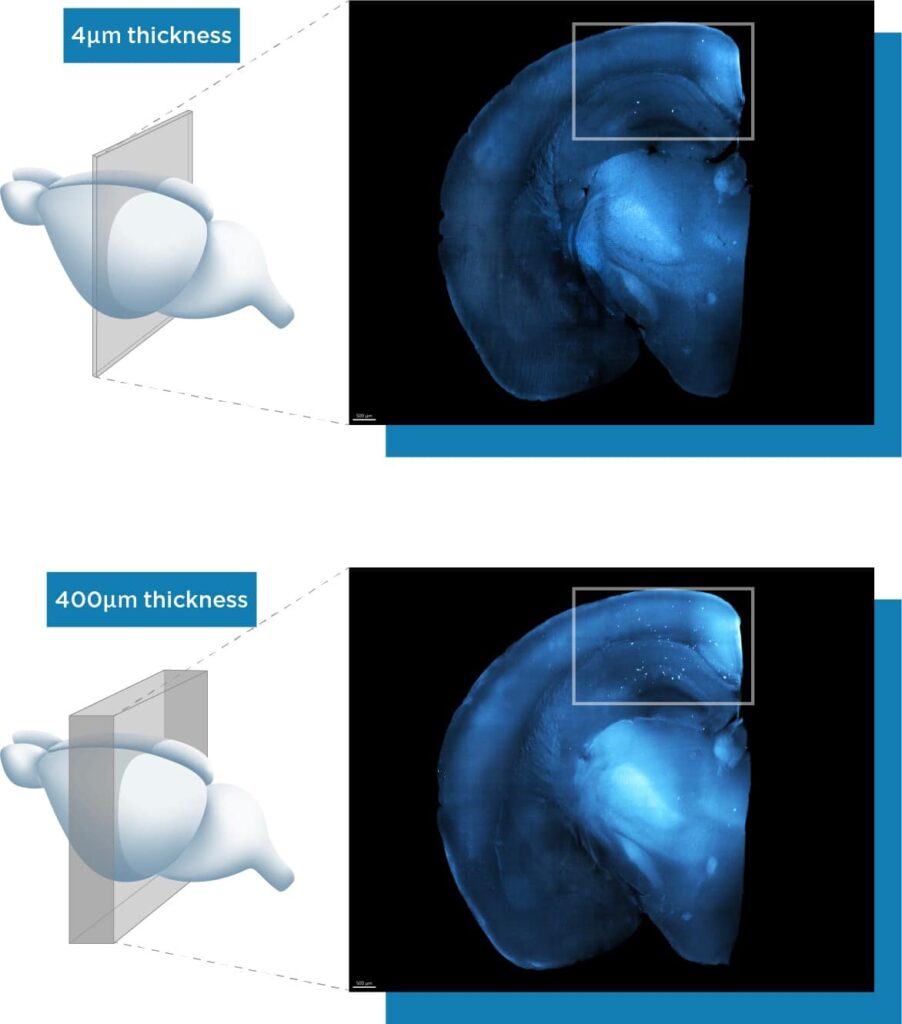
As shown in the case study, traditional tissue slice techniques can miss significant amounts of β-amyloid deposition due to slice thickness limitations, causing plaque quantity and density analysis errors. Nebulum 3D Whole Tissue Imaging can observe minimal protein deposition and prevent missed slice locations to obtain accurate analysis and observations.
Traditional sectioning has its limitations, but the 3D Whole Tissue Imaging technology can reveal complete and minimal protein aggregation during the early stages of AD with small amounts of β-amyloid aggregation. In the late stages of the disease, the technology can also shed light on the relationship and manifestations of β-amyloid and microglia in the brain, helping researchers to unravel the mystery of the role of inflammation in AD.
The Nebulum 3D Whole Tissue Imaging technology is a powerful tool in the fight against AD. It can clarify, stain, stack, and obtain clear and comprehensive stereoscopic tissue images without the need for sectioning. This technology verifies prior experimental results, reduces unnecessary variables and costs, and accurately tests research hypotheses with stunning efficiency. Nebulum Technologies is leading the charge, using this technology to image mouse brains and designated tissues and organs in multiple rodents. And the best news? They’re collaborating with clinicians to expand its applications to human brain and tumor tissues. The battle against AD continues, and hope is on the horizon.
